Breast cancer
Breast cancer is the most common cancer in women in the US, the second leading cause of cancer death in women (after lung cancer), and the leading cause of death in women aged 45 to 55 years.
When detected and treated early, breast cancer is usually curable. Breast cancer deaths have fallen by a third or more over the past three decades. This is partly due to the implementation of screening, as well as timely and effective treatment.
Screening usually detects the disease at an early stage, when the chances of successful treatment are higher. Early detection and treatment of breast cancer improves survival as the tumor can be removed before it metastasizes. In addition, there are treatments that can be used to prevent the development of metastases.
Screening
Μammogram
A mammogram is a low-dose “x-ray” of the breast. It is the best screening test for detecting cancer at an early stage. Some mammograms capture images digitally, offering better clarity.
3D tomosynthesis is a type of enhanced digital mammography that captures multiple images of the breast and helps detect abnormalities that may be hidden by overlapping tissue. In addition, small details become visible, helping the radiologist determine which lesions are benign (not cancer) and which lesions need further investigation.
What if the mammogram is abnormal?
If the mammogram is abnormal, further tests will likely be needed. In some cases, a breast biopsy (in which a small amount of tissue is removed for examination) is required.
What if the mammogram is normal but there is still “something abnormal” in the breast?
Some types of breast cancer may not be detected on mammography, especially in the early stages. For this reason, it is important to inform the attending physician if any change is observed in the breast, even if the mammogram is normal.
When should mammogram screening begin?
In general, the benefit of screening is that it can detect breast cancer early when it is most likely to be treatable. However, there are also disadvantages to control. For example, there may be “false positives” (when test results suggest cancer and lead to additional tests that ultimately do not detect cancer).
There is also the chance that screening will detect cancer that is developing so slowly that it may never cause health problems or become life-threatening. Sometimes the treatment of these types of cancer can cause serious side effects, without ensuring a prolongation of survival.
For women at average risk, that is, those who do not have a gene that increases the risk of breast cancer or close relatives who had breast cancer at a young age, screening is recommended from age 40.
Screening recommendations may be different for women who are at higher risk of developing breast cancer. This category includes women with:
- two or more relatives with a history of breast or ovarian cancer,
- with a relative with a history of breast cancer before the age of 50,
- relatives with a history of two cancers (breast and ovarian or two independent in the breast),
- male relatives with a history of breast cancer.
- Younger women should be considered
Women aged 20-39 are recommended to see a qualified physician for a clinical breast examination every 3 years. The chance of cancer is very low in women under the age of 20 and gradually increases with age. From the age of 20, optional monthly breast self-examination is recommended for women.
How often should a mammogram be done?
Recommendations for women at average risk are for a mammogram every year. Recommendations are different for women who are at higher risk of developing breast cancer.
When can mammogram screening be stopped?
Mammography screening for women over 65 should be based on their health status and especially whether or not they suffer from other serious illnesses. Advanced age alone is not a reason to stop regular mammography. As long as a woman is in good health and able to receive treatment for breast cancer, she should continue to be screened on a regular annual basis.
Breast ultrasound
Ultrasound is not recommended as a routine test for women at average risk for breast cancer.
women with dense breasts (a term used to describe the appearance of breast tissue on imaging) have a slightly increased risk of breast cancer. The high density of the breast can make it difficult to interpret the mammogram. In this case, an ultrasound may be recommended in addition to the mammogram.
Breast MRI
MRI is not routinely used to screen for breast cancer in most women. It can help diagnose breast cancer in the following cases:
- Breast cancer screening for young women, especially those with dense breasts, is at a very high risk of developing cancer (such as those with a very strong family history of breast cancer or a genetic mutation such as BRCA1 or BRCA2).
- Evaluation for breast cancer in women who have been diagnosed with axillary lymph node cancer but no breast cancer has been detected on physical examination or mammography.
- Evaluation of a woman with newly diagnosed breast cancer with extremely dense breasts on mammograms.
Breast Cancer – Diagnosis
Cancer can be detected when a lump or other change in the breast or armpit is noticed by the woman herself or her doctor. In addition to a lump, other abnormal changes may be:
- skin resembling the peel of an orange
- change in breast size or shape;
- retraction (pulling in) of the nipple, when it was previously pointed out
- or discoloration of the skin of the breast, not related to infection or skin conditions such as psoriasis or eczema
To evaluate a lump or change, a mammogram or breast ultrasound is usually recommended. If imaging tests are suspicious, a breast biopsy is usually recommended. A suspicious lump should never be ignored, even if a mammogram is negative. Up to 5-15% of breast cancers are not visible on a mammogram.
Breast biopsy
If breast cancer is suspected, the next step is to examine part of the lesion under a microscope to confirm the diagnosis. Taking the tissue (biopsy) is done with a needle with the help of an imaging test (such as a mammogram, ultrasound, or MRI).
Fine-needle aspiration may be sufficient to establish a diagnosis of breast cancer, although a larger-gauge needle biopsy is often preferable as it provides a larger/adequate sample to better determine certain characteristics of cancer.
Types of Breast Cancer
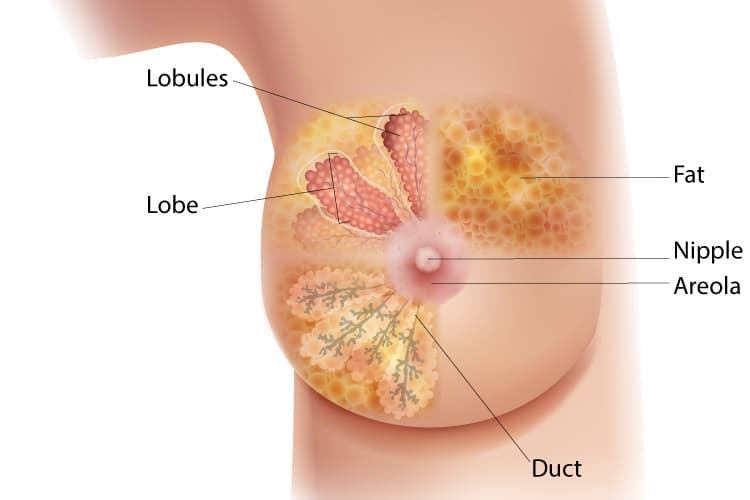
Although there are several different types of cancer, they can be roughly divided into two broad categories. Intraductal (“in situ”) and invasive cancer.
Intraductal (in situ) cancer
In this type, the cancer cells are confined to the breast gland, ducts, and lobules, without spreading to the surrounding fatty tissue. Ductal cancer does not spread outside the breast. However, it can develop over time into invasive cancer if left untreated.
Invasive cancer
Cancer cells have spread outside the ducts and lobules into the surrounding breast tissue. There are several different types of invasive cancer.
The degree of histological malignancy (grade) (calibration carried out by the pathologist) of a tumor describes how aggressive it is and by extension how fast it grows. The grade of histological malignancy ranges from 1 to 3. Tumors with higher grades of histological malignancy are more likely to need chemotherapy.
Characteristics of breast cancer affecting treatment choice.
Breast cancer should be screened for the presence of two types of proteins: hormone receptors (estrogen (ER) and progesterone receptors (PR)) and HER2 (for invasive cancers). These proteins are important for treatment selection. These tests are performed by the pathologist.
Has Breast Cancer Spread?
After the diagnosis of breast cancer is documented, the next important questions are:
1. What is the extent of cancer within the breast?
2. Are there signs that the cancer has spread outside the breast (metastasis)?
The extent of cancer within the breast is usually determined by biopsy findings and the results of mammography, ultrasound, and breast MRI.
Cancer can spread outside the breast through the lymph and blood vessels (metastasis).
Metastases may be visible/palpable, cause symptoms (eg bone pain), or may be detected by imaging tests such as computed tomography (CT), bone scintigraphy, and positron emission tomography (PET).
The importance of axillary lymph nodes
One of the first sites of the spread of breast cancer is the lymph nodes of the armpit. These may swell and be palpable. Other times, they are found on ultrasound, mammography, or MRI. Even if the lymph nodes are swollen, the only way to determine if they are cancerous is to examine a section of them under a microscope.
If the lymph nodes have metastasized, further removal of the axillary lymph nodes is performed.
In women with early breast cancer who do not have obvious involvement of the axillary lymph nodes, a procedure called a sentinel lymph node biopsy is performed. In this, tracers are used to mark the lymph nodes to which the cancer would go first (“sentinel lymph nodes”). These lymph nodes are removed and examined pathologically.
The main advantage of the sentinel lymph node procedure is that it provides important staging information while causing fewer problems, such as arm swelling (lymphedema) than a more extensive axillary lymphadenectomy.
Whether or not lymph nodes are involved is one of the most important factors in determining the long-term outcome (prognosis) of cancer and often guides treatment decisions.
21 gene testing (Oncotype DX)
A genetic test called the Oncotype DX Recurrence Score (RS) can be performed on tumor tissue to help make decisions about chemotherapy, especially for women who are hormone receptor-positive, HER2 negative, and have free lymph nodes. The test examines 21 different genes to assess the genetic makeup of the tumor and provides a score to help predict the likelihood of recurrence.
The oncologist uses this information, along with other information about the patient and the tumor, in making decisions about the need for chemotherapy.
Breast Cancer – Staging
Oncologists use a staging system (TNM) to describe the stage of cancers. “T” refers to the primary tumor, “N” to the regional lymph nodes, and “M” indicates the presence or absence of metastases in other organs.
The stages range from I (less advanced) to IV (more advanced). Stage 0 concerns patients with intraductal cancer only. The “stage” of the cancer is an indication of whether and how far it has spread. Grade and stage are often confused by patients, but they are different concepts.
Staging is done by physical examination, imaging tests, and pathologic examination.
Treatment
The treatment must and can be individualized and is based on several factors:
- the histological type of cancer
- the invasive capacity of the cancer cell
- presence of infiltrated lymph nodes
- tumor size at the time of diagnosis
- distant metastases
- presence of hormone receptors
- presence of HER2 protein
- the general state of health of the woman
Optimal management requires collaboration between physicians of various specialties: surgeons (breast cancer and plastic surgeons), radiologists, pathologists, pathologic oncologists, and radiation oncologists.
Each woman can and should discuss the available treatment options with her doctors to determine which treatment is best for her.
Breast cancer treatment is based on:
- Surgery. The surgery aims to remove the cancerous mass, to preserve as much of the breast as possible when this is oncologically possible, and finally to remove the axillary (local) lymph nodes where it is oncologically required and up to the required level. The earlier extensive (radical) mastectomies that essentially mutilated women without improving the outcome of the disease have now been abandoned. Today cancer surgeries are targeted interventions. From an oncological point of view, they are radical while simultaneously aiming to preserve the organ. The lymph node cleansing of the armpit and the extent of removal is shaped by the sentinel lymph node finding of the specific type and size of the tumor. In several cases, during the performance of the mastectomy, special care is taken in collaboration with a plastic surgeon to restore the shape and size of the breast.
- Radiation therapy. Radiation therapy is always applied in cases of breast conservation after the removal of a cancer such as in lumpectomies. Depending on the stage of the disease, it will sometimes need to be done in women who have had a total mastectomy.
- Chemotherapy or hormone therapy. It is almost always done after surgery for an invasive cancer. Its type depends on the existence or not hormone receptors on the surface of cancer cells (positive hormone receptors) and the menstrual state of the patient.
What’s new in the treatment of breast cancer?
The newest data in the treatment of cancer comes from the field of molecular biology. Today, there are specific molecular biology laboratory tests that analyze the cells of the removed tumor. They also control the expression levels of 21 genes from the same cancer cells.
Based on tumor gene expression, a patient’s likelihood of benefiting from chemotherapy can be predicted. In addition, the risk of recurrence of the disease is controlled. Patients with a low score (<18) have a low probability of disease recurrence and can avoid chemotherapy by receiving hormone therapy alone.
A significant reduction in breast cancer metastases and recurrences appears to be achieved by administering the therapeutic vaccine, based on the HER2/new oncoprotein, according to a recent study conducted in the USA.