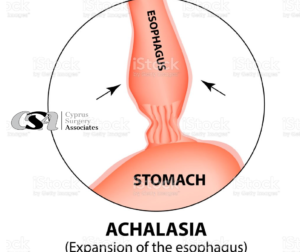
 Achalasia is a swallowing disorder caused by loss of function in the lower esophageal sphincter (the muscular ring at the junction of the esophagus and the stomach). Normally, when people swallow, the sphincter relaxes to allow food and liquid to pass into the stomach. With achalasia, that sphincter does not relax, which causes food to lodging in that area.
Achalasia is a swallowing disorder caused by loss of function in the lower esophageal sphincter (the muscular ring at the junction of the esophagus and the stomach). Normally, when people swallow, the sphincter relaxes to allow food and liquid to pass into the stomach. With achalasia, that sphincter does not relax, which causes food to lodging in that area.
- Achalasia is a rare disorder with about eight to 12 people per 100,000 diagnosed.
- The mean age for the onset of achalasia ranges between 30 to 60 years, with a peak in the forties.
- The disorder is more prevalent in men than women, with a ratio of about 2 to 1.
- Achalasia causes symptoms of coughing, choking, regurgitation, dysphagia, and food retention in the esophagus.
The goal of treatment for achalasia is to decrease the resistance of the esophagus, allowing food to flow through the lower esophageal sphincter (LES).
Why people are afflicted by this sickness is unknown.
Because the sickness is unusual, it’s often difficult to get a correct diagnosis straightaway. Commonly, symptoms are confused with those of hiatus hernia or, just as likely, the sickness can be incorrectly diagnosed as anorexia or bulimia nervosa.
The common symptoms of achalasia
- It is always a problem to swallow food above a certain bite size (bolus).
- You would prefer to stand up during mealtimes and even try to ’jump’ the food down.
- Food becomes stuck in the esophagus unchewed and unprocessed, which creates an urge to be sick. Food vomited in this way comes up whole and undigested. Amongst youths and teenagers, this is easily misdiagnosed as anorexia or bulimia.
- A feeling of cramp in the chest.
- Repeated pneumonia is common.
- Sudden weight loss.
The underlying causes of the symptoms of achalasia
Achalasia is characterized by a disturbance of motor functions both in the inner longitudinal muscle layer of the esophagus and in the lower esophagus sphincter (LES). This means that the forcing muscle layer in the esophagus has stopped working properly, and therefore food travels less efficiently than normal down to the stomach.
Diagnosis
pH test: base pH value >7.
Pressure measurement (e.g. a color manometry): increased pressure in the region of the lower esophagus mouth
Swallow x-ray: widening of the lower esophagus
Gastroscopy: is performed to rule out other causes.
Treatment
Medical treatment
Surgical methods:
- The LES is widened from within with a balloon. This method often has to be repeated and can be unnecessarily painful for the patient. There is also a risk that the esophagus will split, requiring emergency surgery.
- Laparoscopic surgery: the lower part of the esophagus musculature is cut through as far as the mucous membrane. This is done so that the lower esophagus can be widened, and food thus passes more easily (Heller’s myotomy).
- The same as above, but a so-called Fundoplication is performed as well, in which a cuff is fitted around the lower esophagus mouth so that food cannot run back into the esophagus through the now-widened esophagus sphincter. This procedure has been used successfully in Sweden since the 1990s.
A new method is the eroral Endoscopic Myotomy (POEM). In this procedure, the cutting of the lower part of the esophagus musculature is carried out through an endoscopic technique. The method should mean that it is easier to operate to the individual patient’s requirement and that the patient can be dismissed from the hospital after just a few hours.
However, the method requires careful evaluation. Causing a rupture in the esophagus during the operation would be the most serious complication, and this could lead to infection and the need for further operations. [3]
An operation causes the symptoms to cease in 80 to 90 percent of cases.





