 Summary
Summary
- The pancreas is a gland that secretes digestive enzymes and insulin.
- The symptoms of pancreatic cancer are often vague and common to many other disorders.
- Pancreatic cancer is often only diagnosed in its later stages, which makes it difficult to treat.
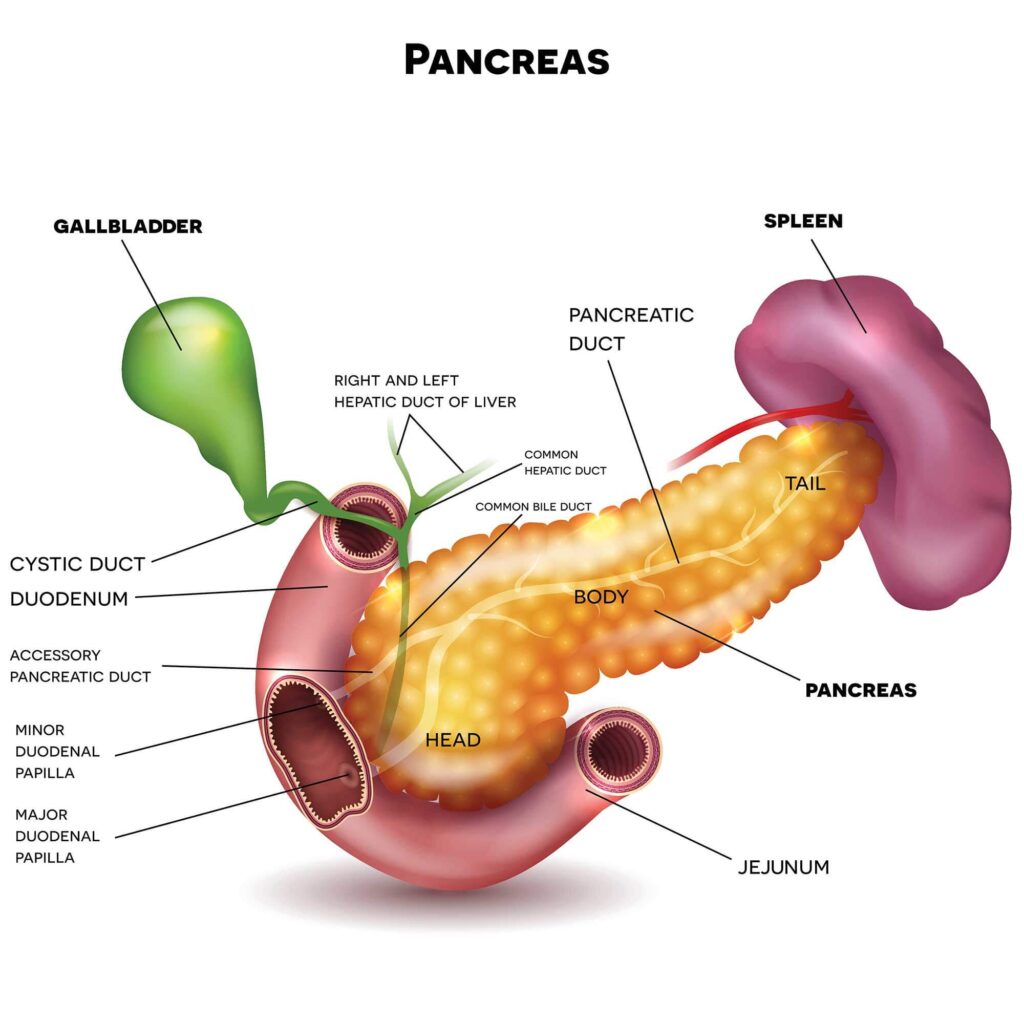
The pancreas is a gland of the digestive system. It is joined to the small bowel by a duct. Pancreatic cancer starts in the cells lining this duct. It then spreads into the body of the pancreas, before invading nearby nerves and blood vessels. If left untreated, it will spread to all the organs in the abdomen. Pancreatic cancer may also enter the lymphatic system and spread to other parts of the body.
The causes of pancreatic cancer are unknown, but smokers are at greater risk. It is more common in people over 65 and relatively uncommon in people under 50 years of age. About 720 Victorians develop pancreatic cancer each year.
Role of the Pancreas
The pancreas has two major roles in the digestive system being that:
- It produces enzymes to help break down food.
- It produces insulin, which controls the amount of sugar in the blood. Problems with insulin production can lead to diabetes.
Risks and causes of pancreatic cancer
Pancreatic cancer is caused by damage to genes, but it is not known exactly why this damage happens. The risk of pancreatic cancer is greater for smokers.
Other risk factors include:
- age – more common in people over the age of 65 years
- genes – inheriting a damaged gene
- diabetes – between 10 and 20 percent of people with pancreatic cancer also have diabetes
- inflammation – chronic inflammation of the pancreas (pancreatitis)
- gastrectomy – having had surgery to remove all or part of your stomach.
Symptoms of pancreatic cancer
Pancreatic cancer symptoms are often vague and can appear similar to those caused by other, less serious conditions. This means that pancreatic cancer is often not diagnosed until it is quite advanced.
Some of the common symptoms may include:
- persistent pain in the abdomen
- loss of appetite
- feeling sick (nausea)
- weight loss
- change in your bowel habits (diarrhea or constipation)
- severe back pain, in some cases.
If your bile duct is blocked, you may also have:
- yellowing of the skin and eyes (jaundice) and itchy skin
- dark urine
- pale feces (bowel motions or poo).
Remember that pancreatic cancer is rare. If you have one of these symptoms, it is likely to be due to something else. However, see your GP (doctor) if you have any symptom that persists for more than two weeks.
Diagnosis of pancreatic cancer
If pancreatic cancer is suspected, your doctor will refer you for tests. These may include:
- Blood tests – these check how well your liver and kidney are working and measure for a protein known as CA19.9. Pancreatic cancer often sends CA19.9 into the blood. It is not used to diagnose pancreatic cancer, but it gives your doctor important information.
- Computed tomography (CT) scan – a special X-ray is taken from many different angles to build a three-dimensional picture of your body. A dye may be injected to further highlight internal organs.
- Magnetic resonance imaging (MRI) – this is similar to a CT scan, but uses magnetism instead of X-rays to build three-dimensional pictures of your body.
- Ultrasound – sound waves create a picture of your pancreas.
- Endoscopy (also called endoscopic retrograde cholangiopancreatography, ERCP) – a thin telescope is inserted down your throat to allow the doctor to see inside your digestive system. This device may also be used to inject dye into the pancreas and bile duct to allow images of these organs to appear on X-ray pictures.
- Laparoscopy – the internal organs are examined with an instrument inserted into the abdomen through a small cut.
- Tissue biopsy – a small sample of the pancreas is removed with a needle and examined in a laboratory.
- Positron emission tomography (PET) scan – an injection with a glucose solution containing a very small amount of radioactive material is given. The scanner can ‘see’ the radioactive substance. Cancerous cells show up as ‘hot spots’ – areas where the glucose is being taken up.
These tests can also help your doctor find out if your cancer has spread. Cancer may have spread into blood vessels or lymph nodes near the pancreas, or into organs further away, like the liver or the lungs. This is called ‘secondary cancer’ or metastasis. The tests you have will help your doctors decide the best treatment for you.
Test results can take a few days to come back. It is very natural to feel anxious waiting to get your results. It can help to talk to a close friend or relative about how you are feeling. You can also contact the Cancer Council and speak with a cancer nurse on 13 11 20.
Treatment of pancreatic cancer
Treatment for pancreatic cancer depends on your age, general health, the size and location of the cancer, and whether it has spread to other parts of the body. You may receive one type of treatment or a combination.
Generally, options include:
- Surgery – is used when cancer has not spread beyond the pancreas. Cancer and part of the pancreas and part of the small bowel are removed in an operation called ‘Whipple’s resection’. Some of the bile ducts, gall bladder, and stomach may also be removed. This is major surgery and you need to be fit enough to have it.
- Chemotherapy – anti-cancer medications (either tablets or injections into the veins) may be used after surgery. The drugs work by stopping cancer cells from growing and reproducing. Chemotherapy may be given with surgery or alone to help control the symptoms of advanced cancer.
- Radiotherapy – the use of X-rays to target cancer cells may be used after surgery to destroy any cancer cells that might remain in the body. Radiotherapy can also be used as the main treatment when surgery is not possible, in combination with chemotherapy.
- Complementary and alternative therapies – it’s common for people with cancer to seek out complementary or alternative treatments. When used alongside your conventional cancer treatment, some of these therapies can make you feel better and improve your quality of life. Others may not be so helpful and in some cases may be harmful. The Cancer Council Victoria booklet called Understanding Complementary Therapies can be a useful resource.
All treatments have side effects. These will vary depending on the type of treatment you are having. Many side effects are temporary, but some may be permanent. Your doctor will explain all the possible side effects before your treatment begins.
Options may include:
- Endoscopic treatment – cancer may cause jaundice because it is blocking the bile duct. Endoscopic surgery relieves the pressure by inserting a metal or plastic tube into the bile duct to keep it open. Similar treatment can relieve a section of the small bowel if the cancer is pressing on it.
- Surgery – a blockage in the small bowel can be bypassed by a surgical procedure that attaches a loop of the bowel directly to the stomach.
- Tablets – there may be a lack of pancreatic enzymes to properly digest fats, which results in diarrhea. Tablets containing these enzymes can control this symptom.
- Pain-relieving medication – oral medication is usually given to control pain, but if the pain is particularly severe, medication can be injected into the nerves of the back.
When a cure isn’t possible
If cancer has spread and it is not possible to cure it with surgery, your doctor may still recommend treatment that focuses on improving quality of life by relieving the symptoms (this is called palliative treatment). This can help make you feel better and may allow you to live longer. The Cancer Council Victoria booklet called Living with advanced cancer may be helpful to read.
References
- Cancer in Victoria, statistics and trends, Cancer Council Victoria.
- Pancreatic cancer, Cancer Research UK.
- Bahra M, Jacob D 2008, ‘Surgical palliation of advanced pancreatic cancer
- Hamada, S, Shimosegawa, T 2011, i Pancreatology, vol. 11, (suppl 2), pp. 14-19.
- NCCN Guidelines for Patients, Pancreatic Cancer, National Comprehensive Cancer Network.
- Pancreatic cancer, The American Cancer Society.
[/vc_column_text]
References
- Cancer in Victoria, statistics and trends, Cancer Council Victoria.
- Pancreatic cancer, Cancer Research UK.
- Bahra M, Jacob D 2008, ‘Surgical palliation of advanced pancreatic cancer
- Hamada, S, Shimosegawa, T 2011, i Pancreatology, vol. 11, (suppl 2), pp. 14-19.
- NCCN Guidelines for Patients, Pancreatic Cancer, National Comprehensive Cancer Network.
- Pancreatic cancer, The American Cancer Society.
[/vc_column_text]






 Summary
Summary